Pathology
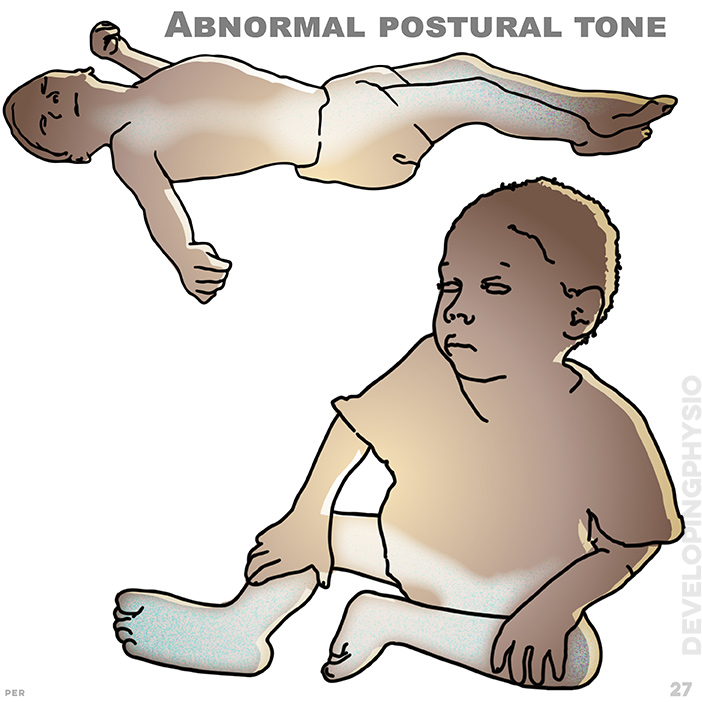
27. Abnormal postural tone: abnormal movement patterns reinforce tonal issues and poor quality posture and movement. tone may range from high to low and much in between
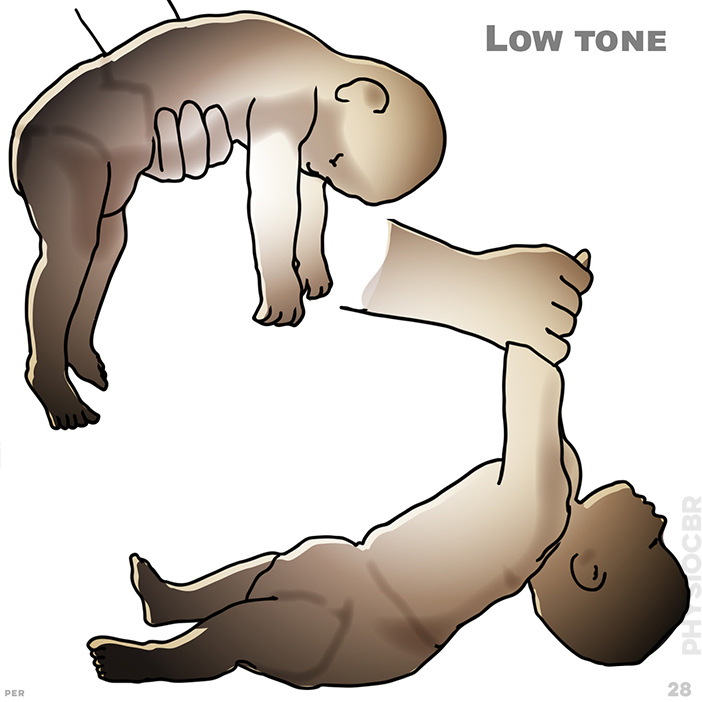
28. Low tone: floppy limbs with reduced muscle activity. low postural tone makes anti-gravity postures difficult
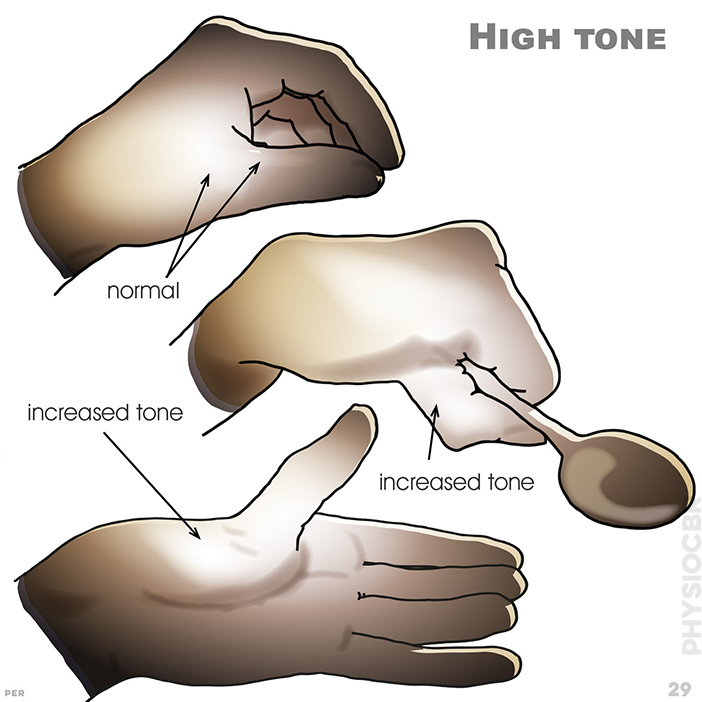
29. High tone: a degree of adduction and flexion is typically found in all limbs. showing typical examples of increased tone
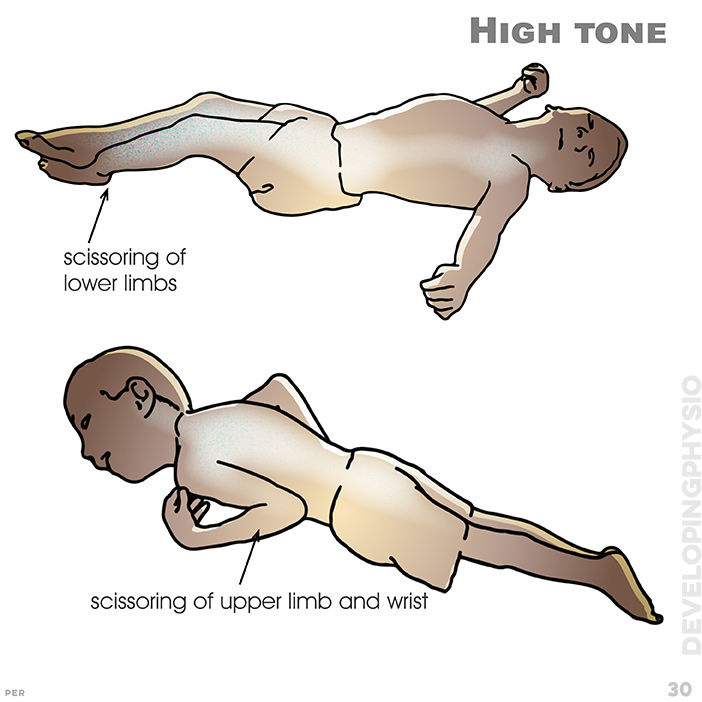
30. High tone: showing scissoring of lower limbs and scissoring of upper limb and wrist
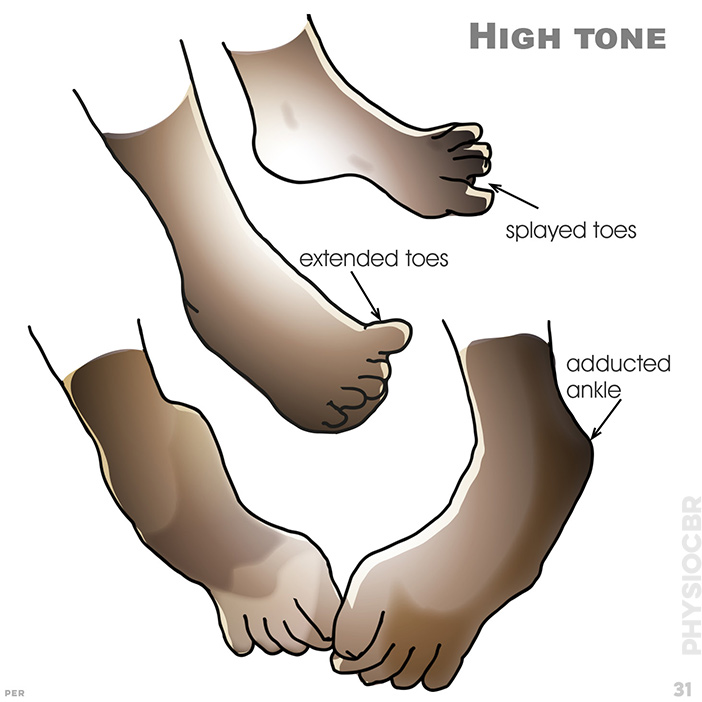
31. High tone: showing splayed toes, extended toes and adducted ankle

32. High tone: prolonged increased muscle tone leads to contractures and the risk of deformity. hip dislocation is a risk
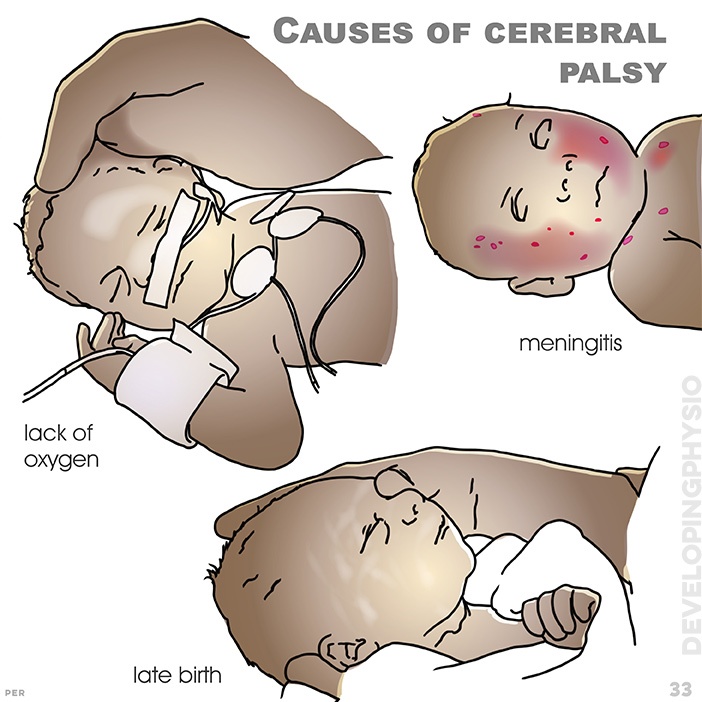
33. Causes of cerebral palsy: the brain may be affected by too little oxygen at birth (normal birth occurs at 40 weeks, so that under 37 or over 42 may have consequence). showing lack of oxygen, meningitis and late birth
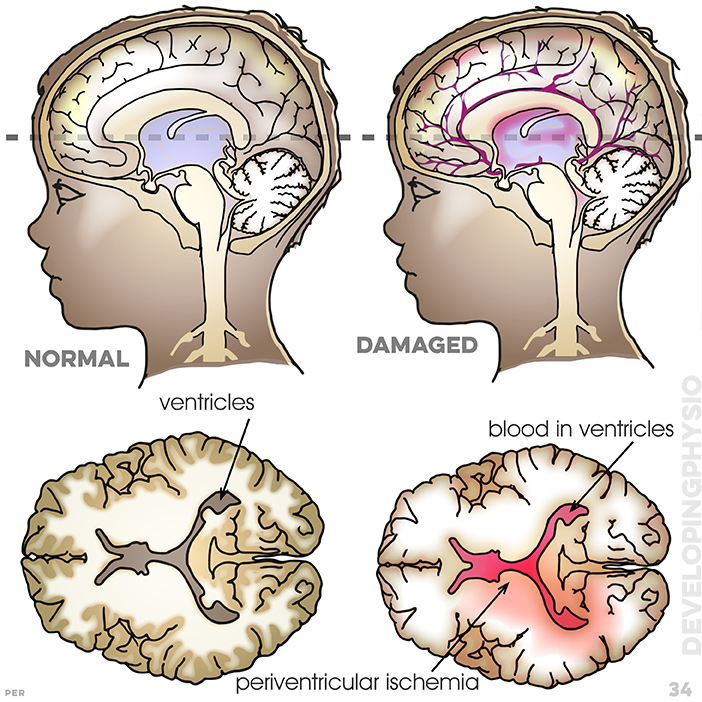
34. Cerebral Palsy: showing ventricles, blood in ventricles and periventricular ischemia
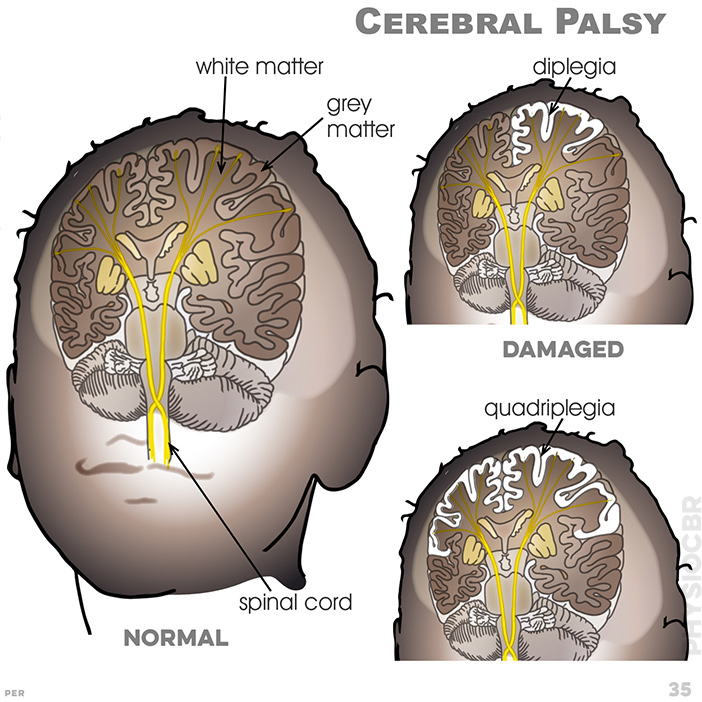
35. Cerebral Palsy: motor cortex; grey matter; white matter; diplegia; quadriplegia
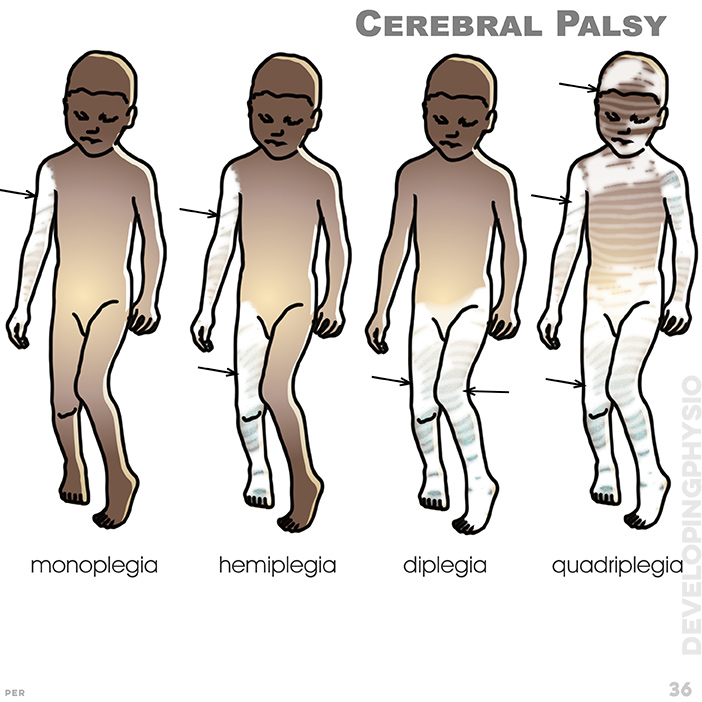
36. Cerebral Palsy: monoplegia : one arm hemiplegia: one side of body; diplegia: involves arms (sometimes trunk), most especially legs. quadriplegia involves all four limbs equally, often arms more than legs
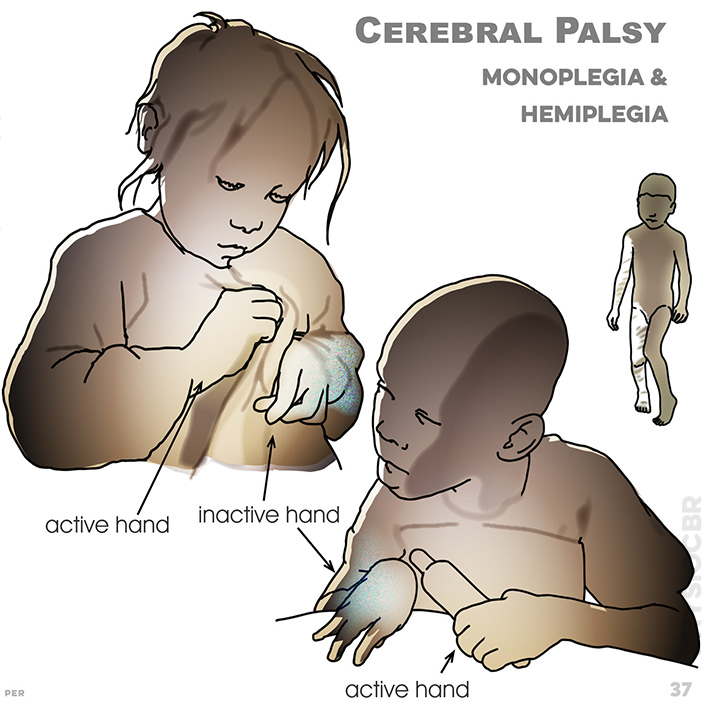
37. Cerebral Palsy, Monoplegia & Hemiplegia: because the motor cortex is affected, movement and sensation can seem quite different on side of the body to the other. showing active and inactive hands
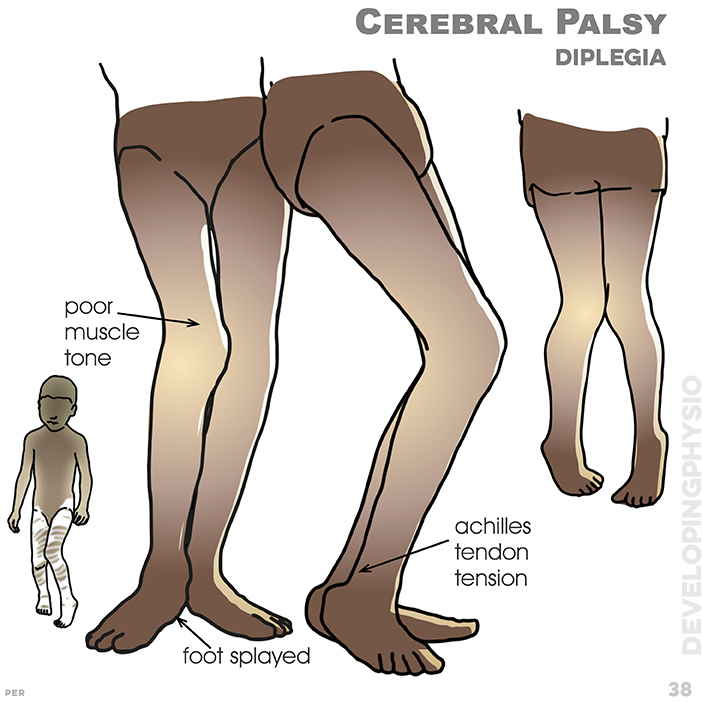
38. Cerebral Palsy, Diplegia: legs often rotate in, pull together and bend at knee, with degrees of bilateral in-toeing and tiptoe gait. showing poor muscle tone and foot splayed, achilles tendon tension
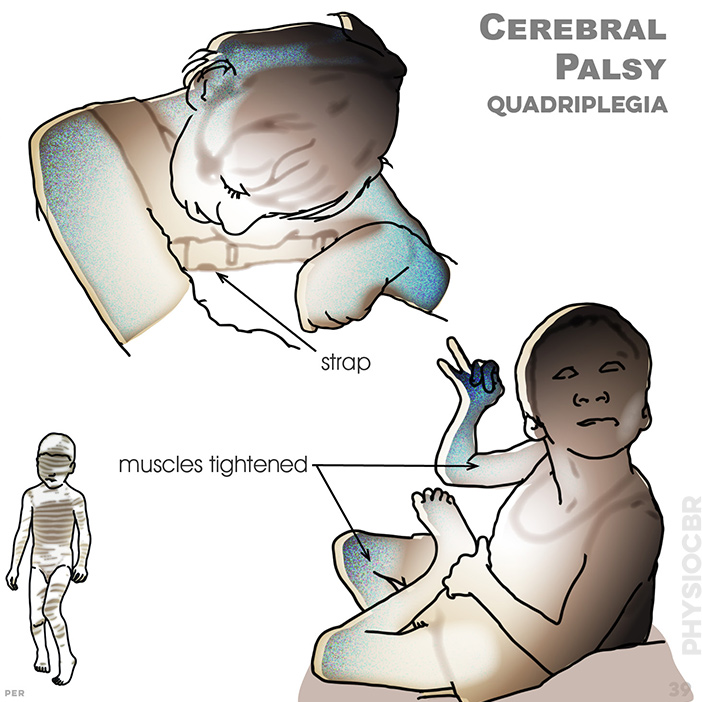
39. Cerebral Palsy, Quadriplegia: common additional impairmen or ts include epilepsy, feeding difficulty, sleep problems and incontinence. typically muscles are tightened or full body support is required (in wheelchair)
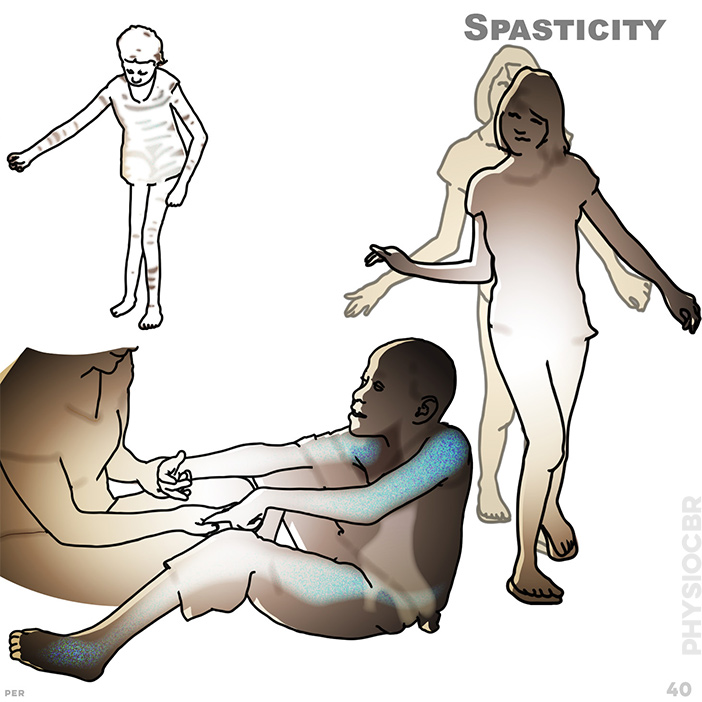
40.Spasticity: increased postural tone limits the patterns of movement, which affects balance and may also lead to contractures and muscle shortening
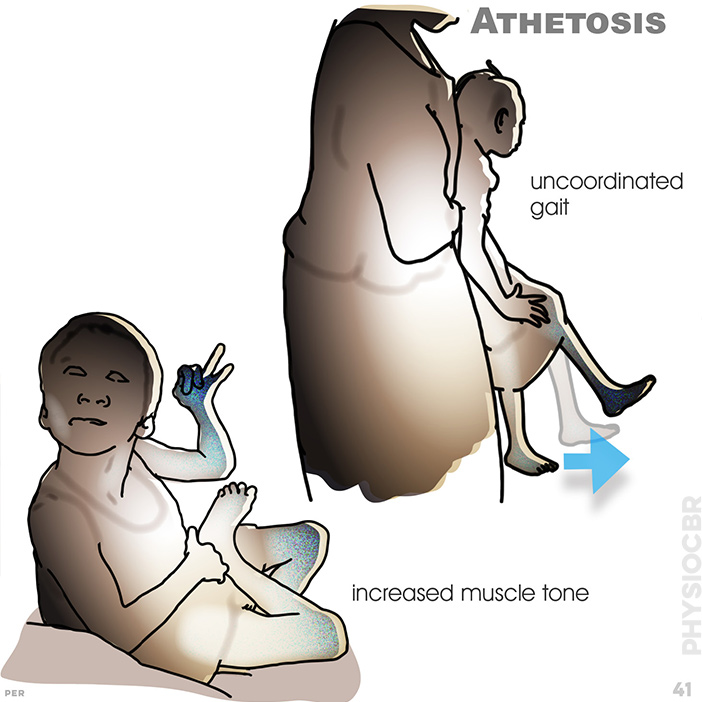
41. Athetosis: poorly co-ordinated, purposeful, large range movements are characteristic. postural tone may range between low and high, but the child usually lacks stability and has difficulty sustaining postural alignment. typical signs are an uncoordinated gait and increased muscle tone. asymmetry may be hypotonic or hypertonic
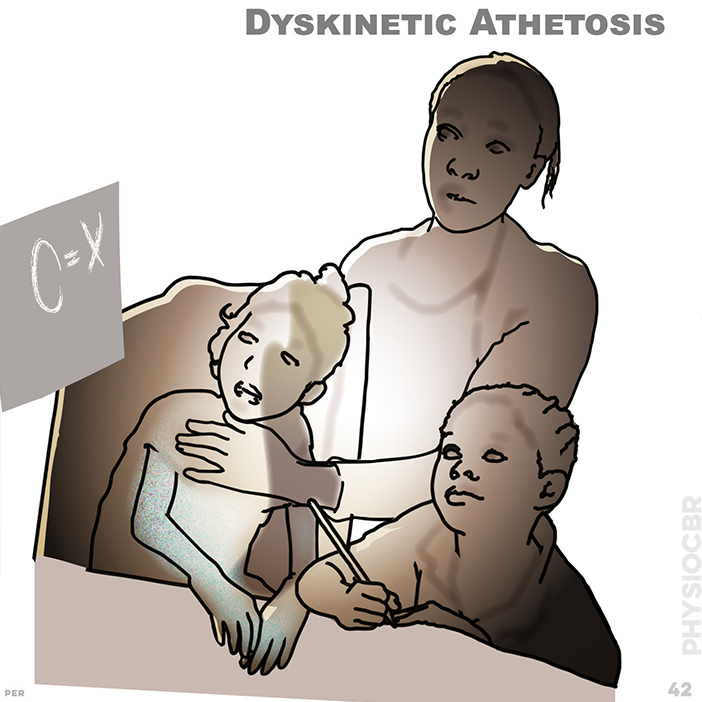
42. Athetosis, dyskinetic: although speech may be impaired by muscles (and suggest learning problems), children with athetosis learn and understand well
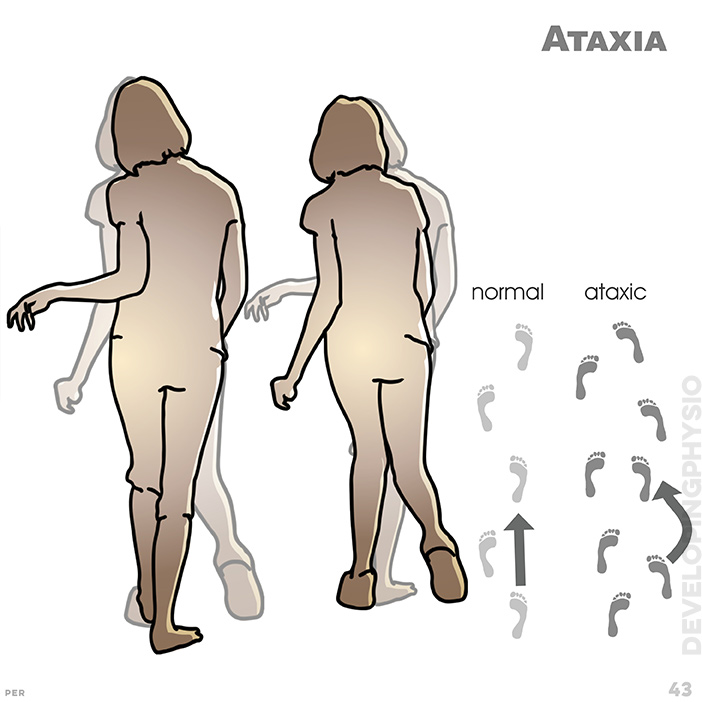
43. Ataxia: Low postural tone, poor function and disturbed balance (like someone who is drunk) are hallmarks of ataxia. Other signs include tremor of intention to move, poor eye tracking and delayed speech. generally poor balance with wide, inward pointing feet/toes and no gait rhythm
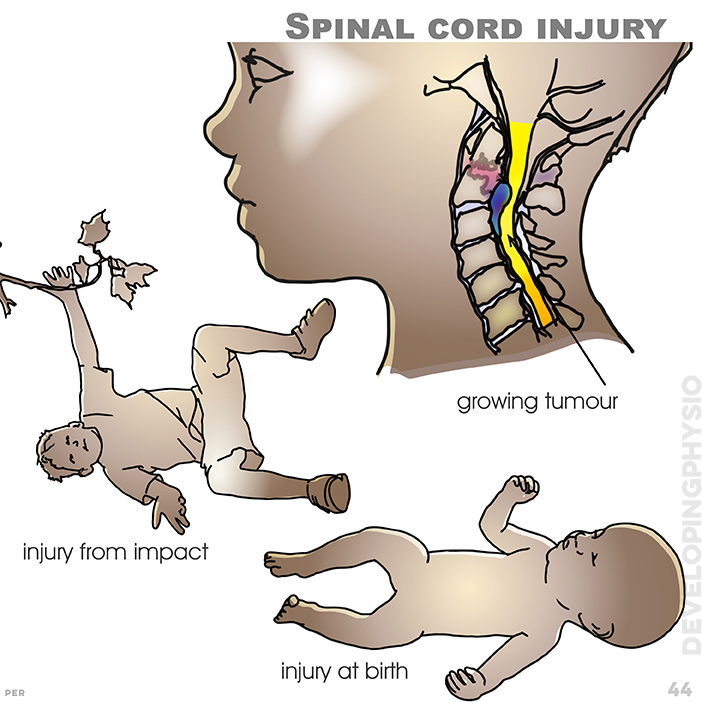
44. Spinal cord injury: showing a growing tumour, injury from impact and injury at birth.
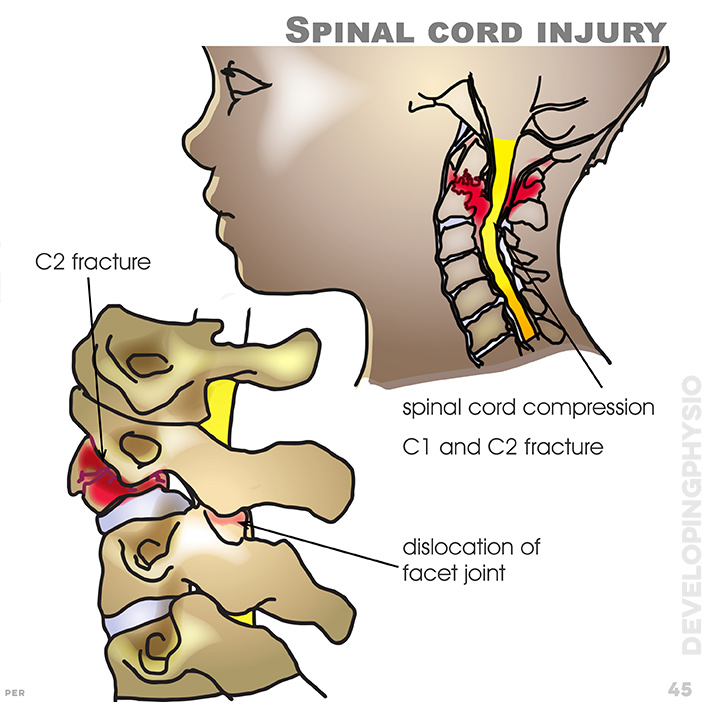
45. Spinal cord injury: Reasons for spinal cord injury include vertebrae dislocation, fracture and tumour. (for full detail, please refer to Spinal Cord module). shown here is spinal cord compression, C2 fracture and dislocation of facet joint (a typical cause might be severe impact from a traffic accident)
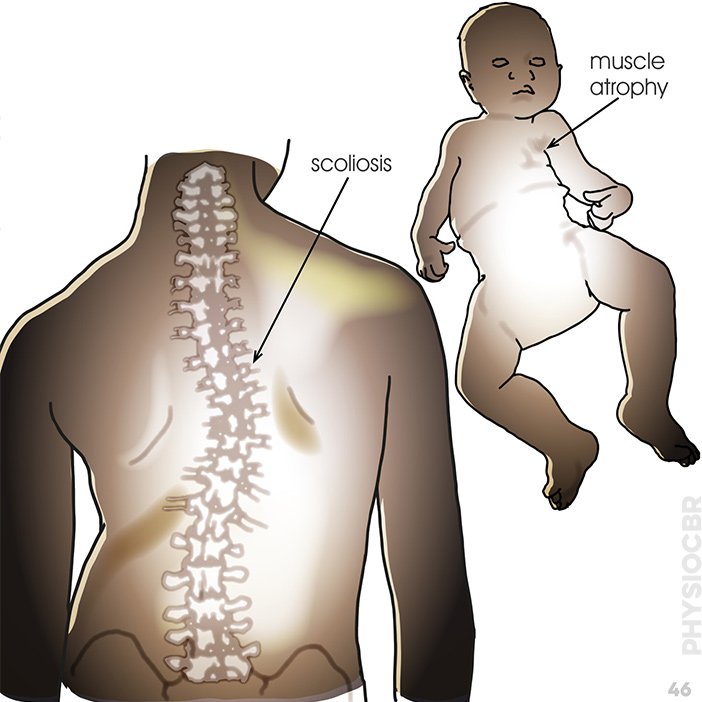
46. Spinal muscular atrophy: Genetic disorder resulting in gradual muscle wasting
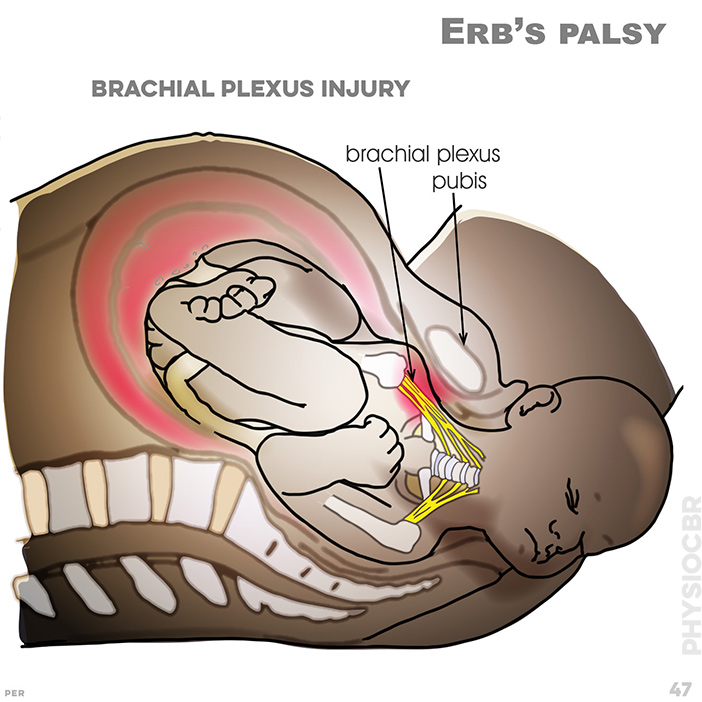
47. Erb’s palsy: Brachial plexus injury caused by shoulder being caught on the pubis bone
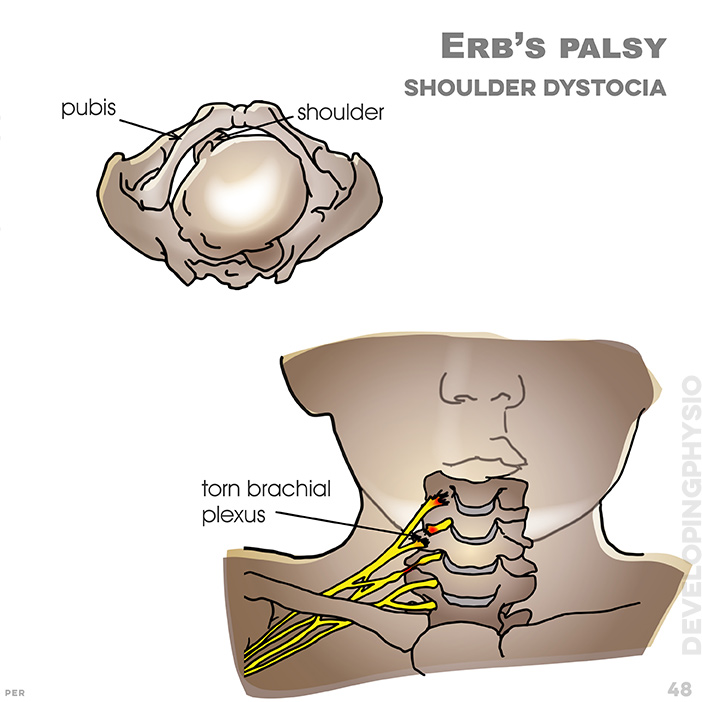
48. Erb’s palsy, shoulder dystocia: During birth, upper limb paralysis can result if there is an injury to the brachial plexus. shows shoulder caught under pubis and (below) torn brachial plexus
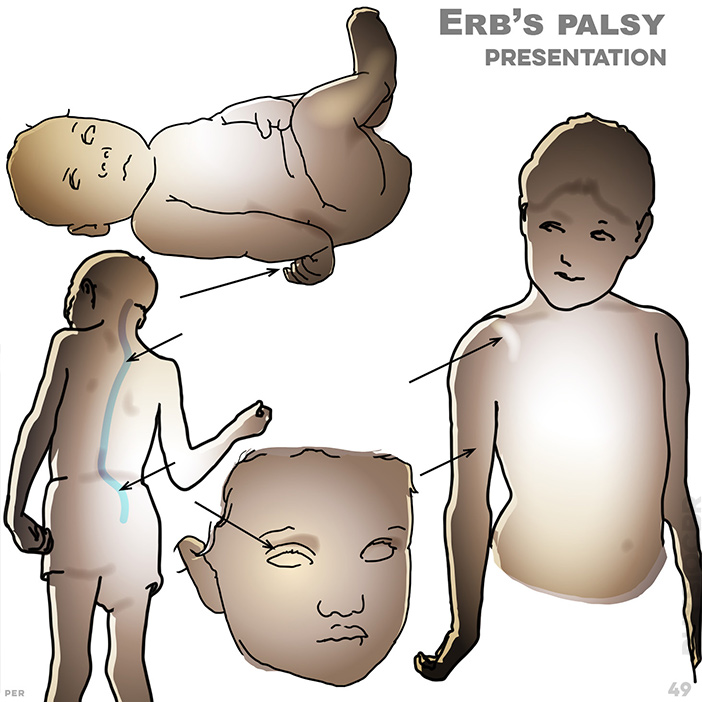
49. Erb’s palsy, presentation: typical signs include: wrist bent backward; lumbar scoliosis; cervical scoliosis; shoulder rotated forward; degree of muscle atrophy; cervical scoliosis; eyelid droops (ptosis)
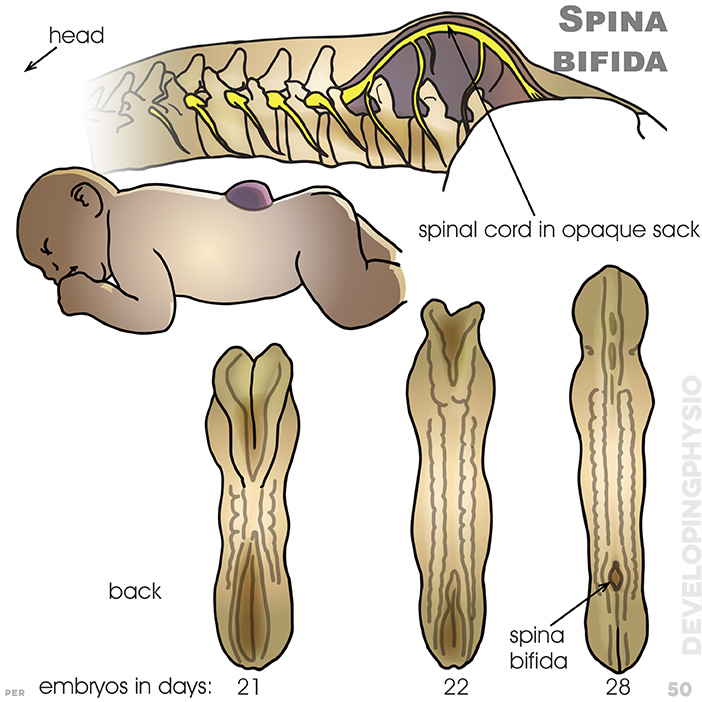
50. Spina bifida: A birth defect in which incomplete closure of the membranes surrounding the backbone and spinal cord causes partial paralysis of legs. shown are spinal cord in opaque sack and the back of an ambryo in days (21, 22, 28)
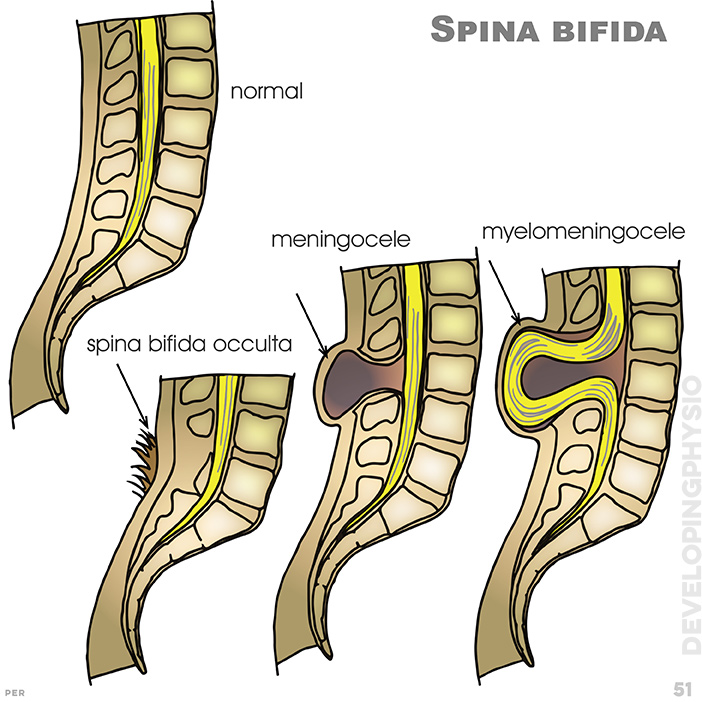
51. Spina bifida: Other symptoms may include hair or dimpling of sacral area. (left to right): spina bifida occulta; meningocele; myelomeningocele; normal
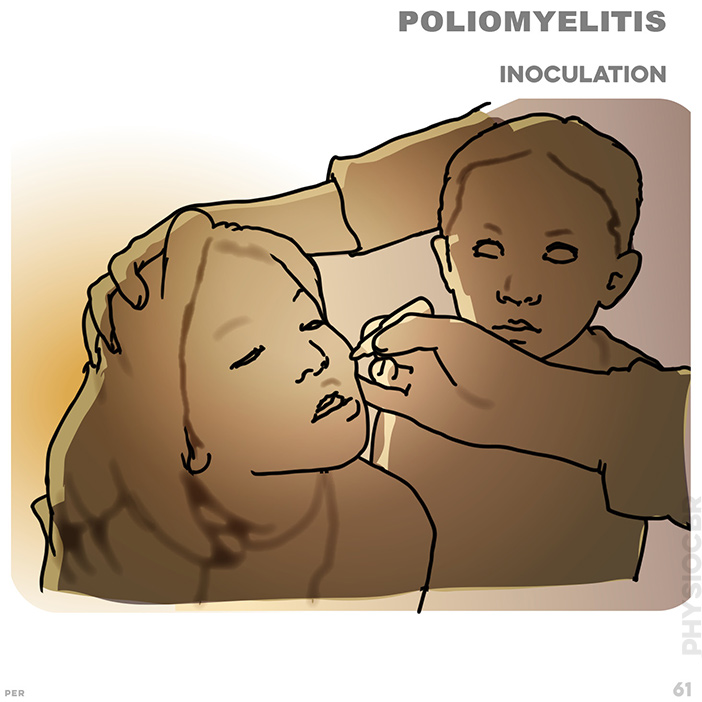
61. Poliomyelitis: walking with minimum aid
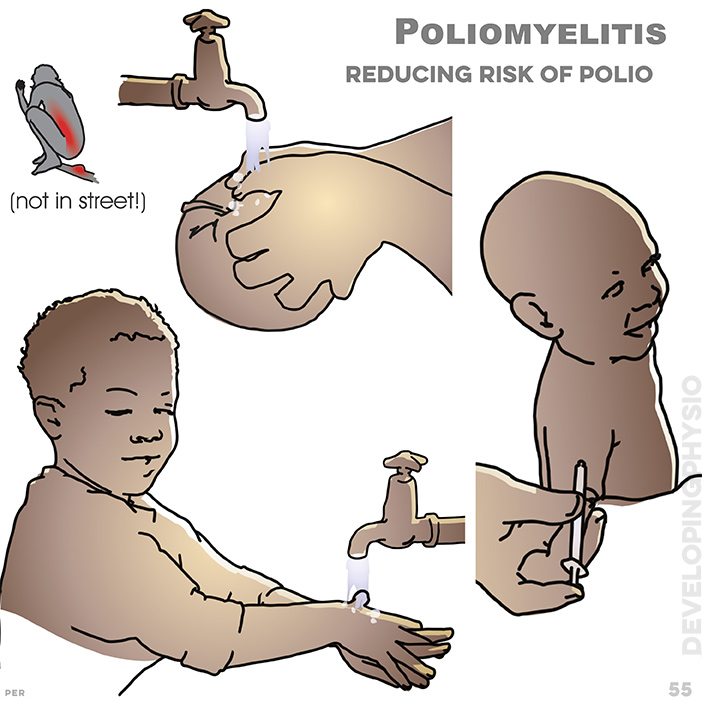
55. Poliomyelitis: Reducing risk of Polio
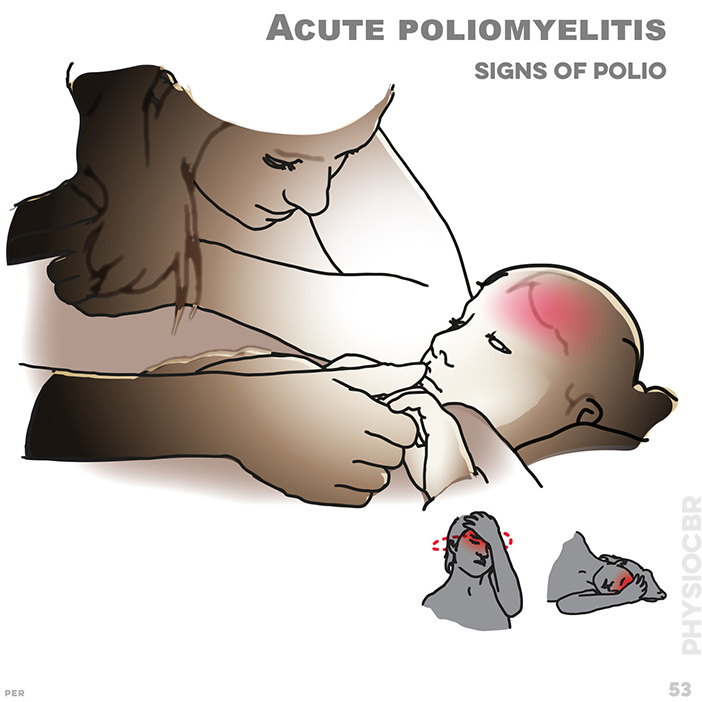
53. Acute poliomyelitis signs: Acute polio results in fever, sore throat, headache and stiffness of the neck, in addition to muscle weakness
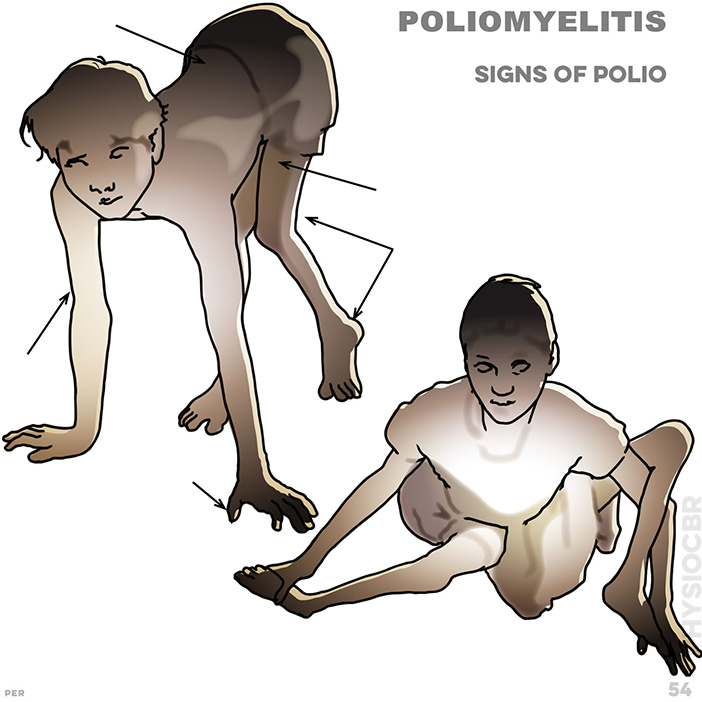
54. Poliomyelitis signs: contracted, tight, corded muscles; muscles that bend or straighten hip; weak posterior arm muscles; weak thumb muscles; weak lumbar muscles
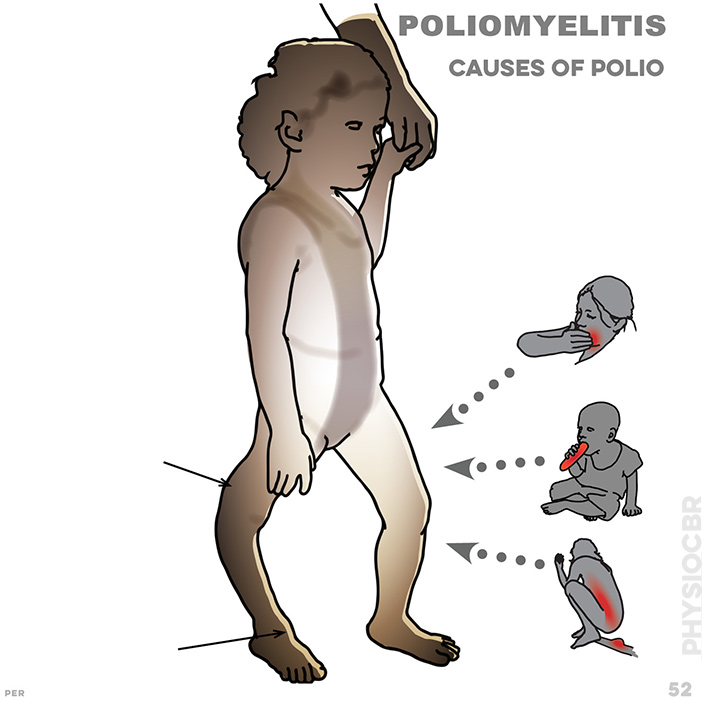
52.Causes of poliomyelitis: the polio virus affects peripheral nerves causing weak muscles. Spread by bad sanitation, contaminated water or food, it is highly contagious. typically affected are muscles that straighten the knee and muscles that lift the foot

56. Gross Motor Function Classification Scale (GMFCS). GMFCS1: confident: confident to walk in public; climbs stairs without railings; runs and jumps. difficult: speed, balance and co-ordination remain limited
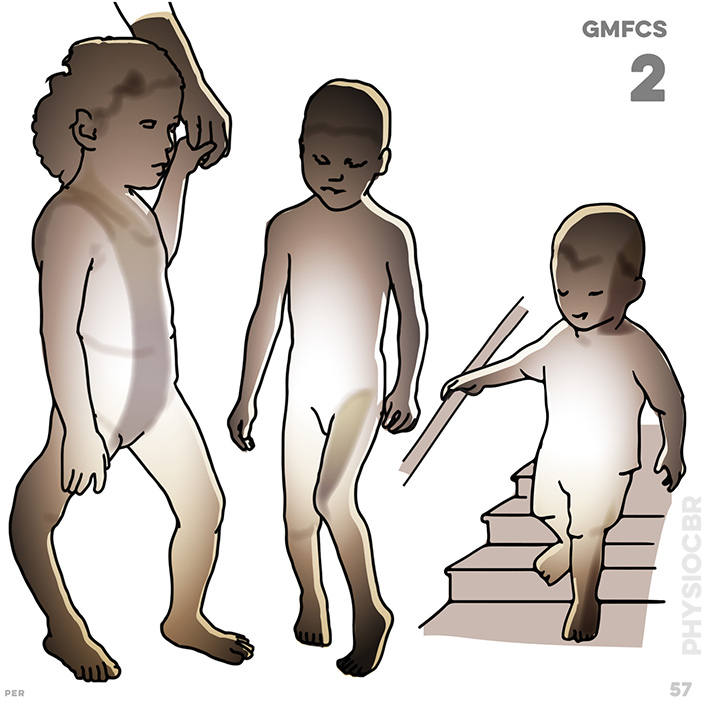
57. GMFCS2: possible: walks on even surfaces; climbs stairs holding railings; . difficult: limited walking on uneven surfaces and slopes and in crowds or confined spaces

58. GMFCS3: possible: walks with assistive mobility device on level surfaces; climbs stairs holding railings; propels wheelchair manually . difficult: needs transport for longer distances and uneven terrain
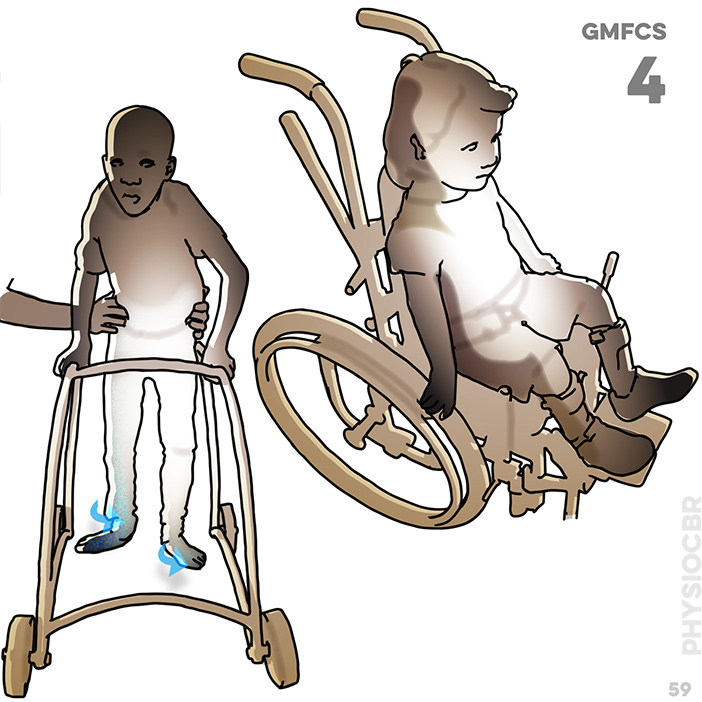
59. GMFCS4: possible: walks short distances with mobility device. difficult: relies on wheeled mobility at home, school and in public places
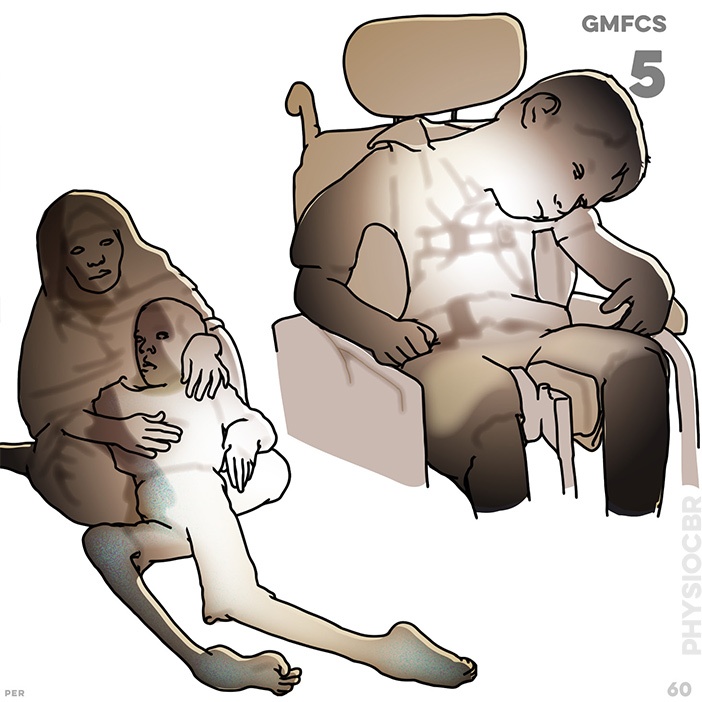
60. GMFCS5: manual wheelchair required for all circumstances; limited ability to maintain posture against gravity and difficulty with leg and arm control